Secondary Glaucoma
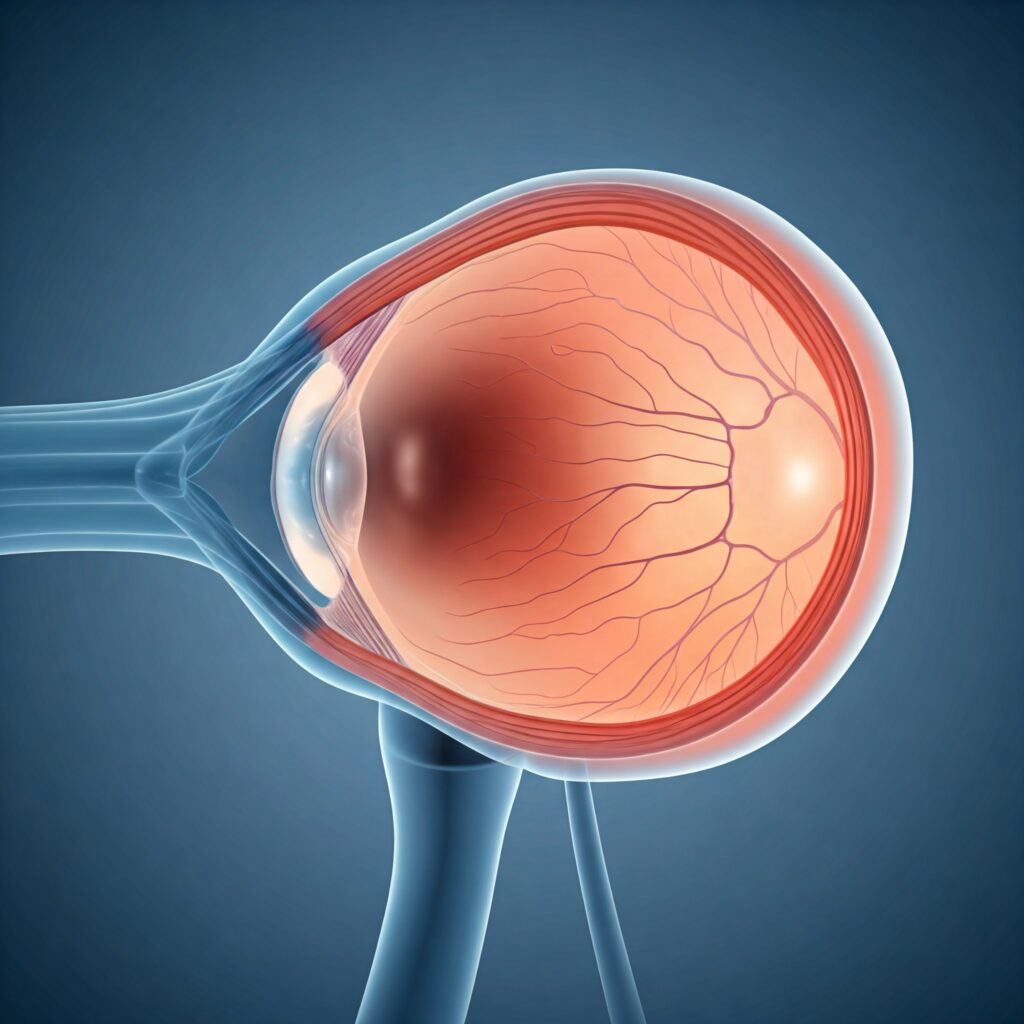
Secondary Glaucoma is a type of glaucoma that arises due to an underlying condition, injury, or medication. Unlike primary glaucomas, which occur without any identifiable cause, secondary glaucomas are a result of other health issues that affect the eye’s drainage system or increase intraocular pressure (IOP).
If left untreated, secondary glaucoma can lead to significant vision loss. There are several types of secondary glaucoma, each with its own distinct cause and mechanism. Let’s explore some of the most common forms.
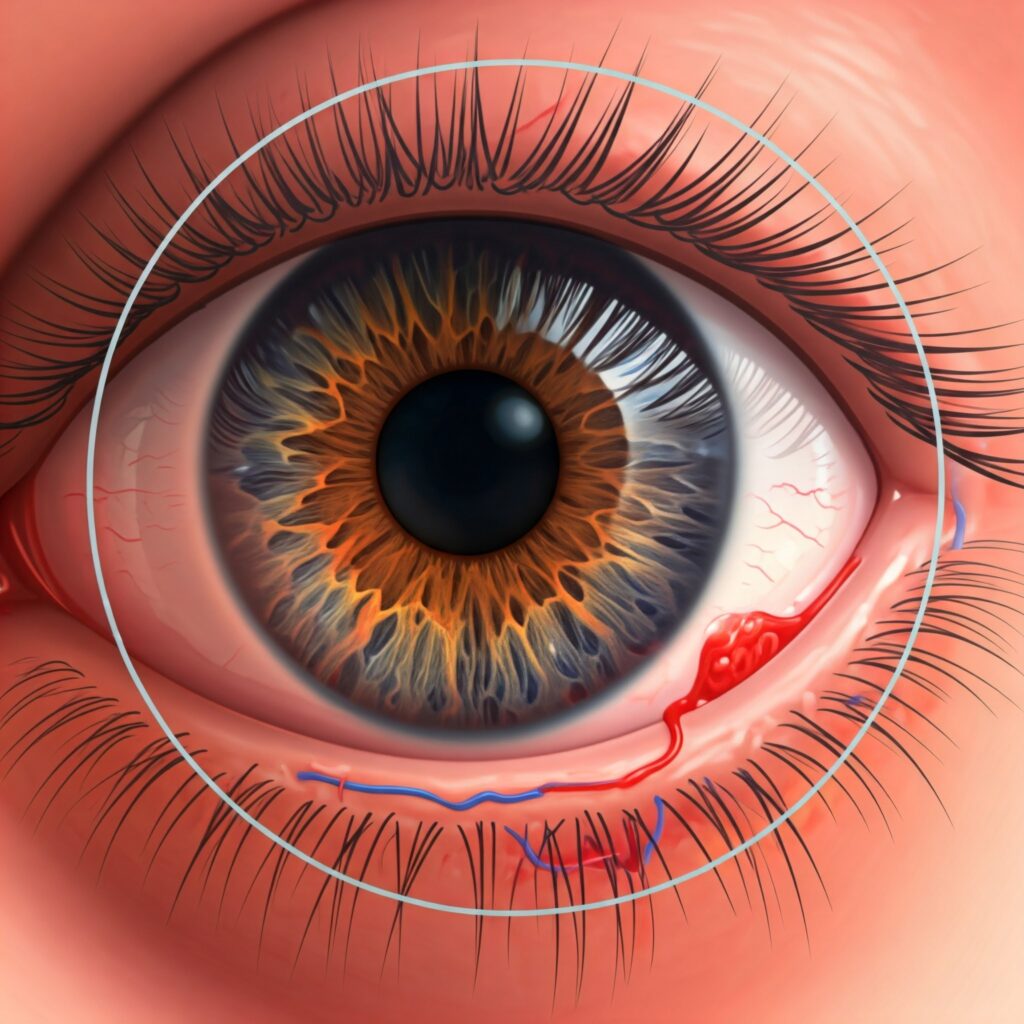
a. Neovascular Glaucoma
Neovascular Glaucoma occurs when abnormal blood vessels grow in the eye’s drainage angle, which leads to blockages and increased IOP. This type of secondary glaucoma is often seen as a complication of conditions like diabetes, especially diabetic retinopathy, or retinal vein occlusion.
Mechanism:
In neovascular glaucoma, the growth of new, fragile blood vessels in the angle of the eye obstructs the flow of aqueous humor, causing a rise in IOP. These abnormal blood vessels can leak and further increase inflammation, exacerbating the condition
Associated Conditions:
The most common underlying conditions associated with neovascular glaucoma include uncontrolled diabetes and retinal vein occlusion, both of which impair normal blood circulation in the eye.
b. Pigmentary Glaucoma
Pigmentary Glaucoma is a type of secondary glaucoma caused by the dispersion of pigment granules from the iris. These granules can accumulate in the trabecular meshwork, which is responsible for draining aqueous humor from the eye. When the meshwork becomes clogged with pigment, fluid drainage is impaired, leading to an increase in IOP.
Cause:
The condition often develops as the iris pigment granules are shed due to the rubbing of the iris against the lens or the trabecular meshwork. This shedding typically occurs in individuals with pigment dispersion syndrome, leading to the development of pigmentary glaucoma

c. Exfoliation (Pseudoexfoliation) Glaucoma
Exfoliation Glaucoma (also known as pseudoexfoliation glaucoma) is associated with the accumulation of fibrillary material, known as exfoliation material, both on the lens and in the drainage angle of the eye. This material is typically found in patients with exfoliation syndrome, a condition where the lens capsule starts to release small fibrillar deposits
- Mechanism:
The fibrillary material that accumulates in the drainage angle obstructs the outflow of aqueous humor, raising IOP. Over time, this can cause progressive optic nerve damage, leading to glaucoma.
Associated Factors:
Exfoliation syndrome is more common in older adults and is often associated with systemic conditions like hypertension or cardiovascular disease
d. Uveitic Glaucoma
Uveitic Glaucoma occurs as a complication of uveitis, which is inflammation of the uvea (the middle layer of the eye). Uveitis can result from infections, autoimmune diseases, or trauma, and it can lead to scarring and damage to the drainage angle of the eye
- Cause:
The inflammation associated with uveitis can obstruct the drainage system of the eye, leading to an increase in IOP. In some cases, the inflammation may cause the trabecular meshwork to become less effective at draining aqueous humor, contributing to glaucoma.
Symptoms:
Uveitic glaucoma is typically accompanied by symptoms of uveitis, such as eye redness, pain, blurred vision, and sensitivity to light.
e. Traumatic Glaucoma
Traumatic Glaucoma is a secondary form of glaucoma that results from an injury to the eye. This could include physical trauma such as a blunt force impact, penetration, or eye surgery. The injury can disrupt the normal functioning of the eye’s drainage system, leading to increased IOP and potential damage to the optic nerve.
Cause:
Injury to the eye can cause a blockage in the drainage angle, either due to bleeding, scarring, or structural damage. In some cases, the trauma may result in a permanent alteration to the eye’s anatomy, leading to long-term glaucoma
f. Steroid-Induced Glaucoma
Steroid-Induced Glaucoma is a type of secondary glaucoma caused by prolonged use of corticosteroids, whether topical, oral, or injected. Steroids can increase IOP in susceptible individuals by affecting the trabecular meshwork, decreasing the eye’s ability to drain fluid efficiently.
Mechanism:
Steroids can cause an increase in the production of aqueous humor and reduce the outflow, leading to elevated IOP. This effect can occur even with short-term steroid use in some people, particularly those with a genetic predisposition
Prevention and Management:
Regular monitoring of IOP is essential for patients on long-term steroid therapy. In many cases, discontinuing or reducing steroid use can help control the elevated pressure.
g. Phacomorphic Glaucoma
Phacomorphic Glaucoma occurs when the lens of the eye swells due to the development of cataracts. This swelling can cause a blockage in the eye’s drainage angle, leading to an increase in IOP.
- Cause:
The cataractous lens becomes larger and more swollen, pushing against the iris and the trabecular meshwork. This impairs the flow of aqueous humor, causing IOP to rise, which can result in acute glaucoma. - Treatment:
The primary treatment for phacomorphic glaucoma is cataract surgery to remove the swollen lens and restore normal drainage.

h. Phacolytic Glaucoma
Phacolytic Glaucoma is another type of secondary glaucoma caused by the leakage of lens proteins into the anterior chamber of the eye, typically occurring in hypermature cataracts. As the cataract degenerates, proteins from the lens leak out and clog the trabecular meshwork, causing an increase in IOP.
- Cause:
In cases of hypermature cataracts, the lens becomes so soft and degenerated that it releases proteins into the eye. These proteins can obstruct the drainage angle, raising the risk of glaucoma.
Treatment:
The treatment for phacolytic glaucoma is typically surgical removal of the cataract. This helps to alleviate the pressure and prevent further optic nerve damage
