Proliferative Diabetic Retinopathy (PDR)
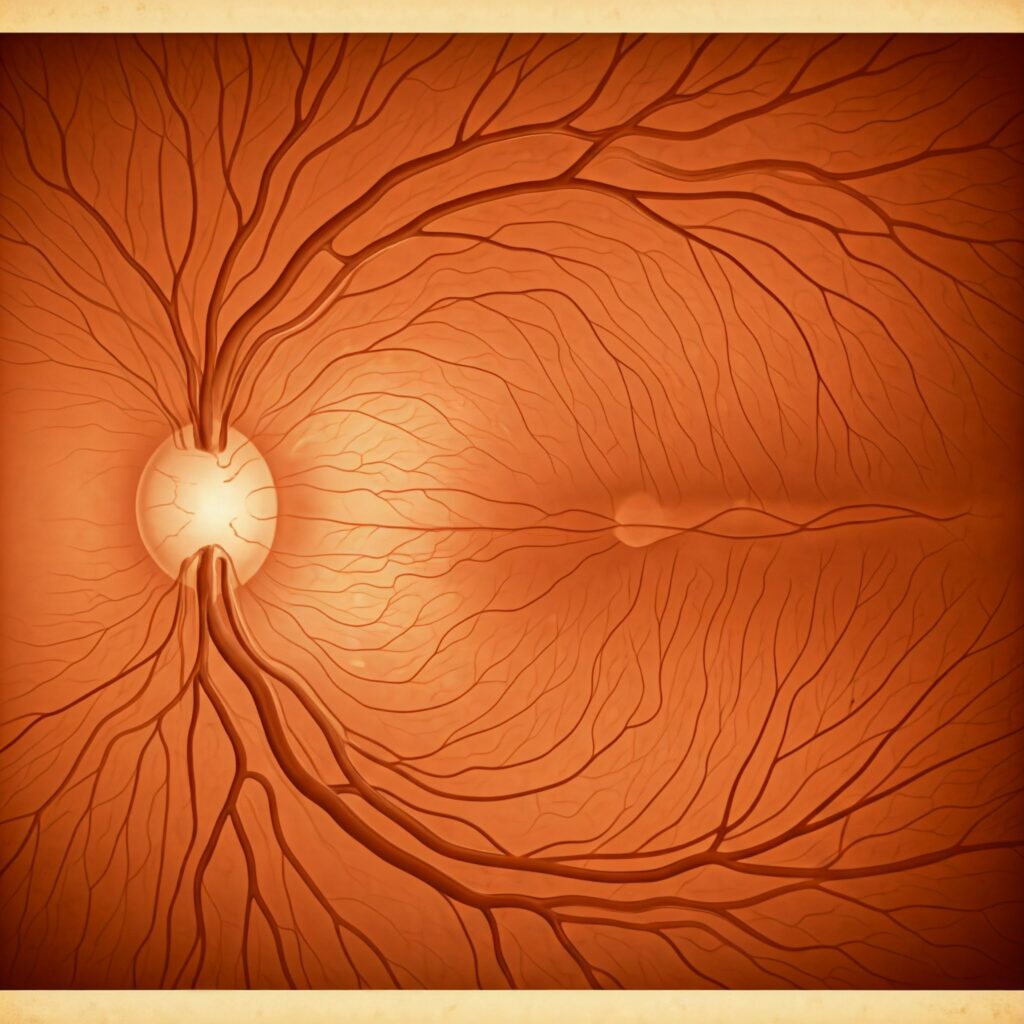
Proliferative Diabetic Retinopathy (PDR) is an advanced stage of diabetic retinopathy, a common complication of diabetes that affects the eyes. In this condition, abnormal blood vessels (neovascularization) develop on the retina or optic disc as a response to oxygen deprivation.
These fragile blood vessels can lead to severe vision complications such as retinal detachment, vitreous hemorrhage, and, in some cases, irreversible blindness.
Signs and Symptoms
Proliferative Diabetic Retinopathy (PDR) may not initially cause noticeable symptoms, especially in its early stages. As the condition progresses, patients might experience:
- Blurred or distorted vision.
- Sudden appearance of floaters or spots in vision.
- Dark or empty areas in the visual field.
- Gradual vision loss, especially in the central or peripheral vision.
Difficulty seeing at night
Causes
The primary cause of Proliferative Diabetic Retinopathy (PDR) is prolonged and poorly controlled diabetes. Elevated blood sugar levels damage the small blood vessels in the retina, reducing oxygen supply (retinal ischemia). In response to this oxygen deprivation, the retina triggers the growth of abnormal blood vessels, marking the onset of Proliferative Diabetic Retinopathy (PDR). Risk factors include:
- Longstanding diabetes (both Type 1 and Type 2).
- Poor blood sugar control.
- High blood pressure (hypertension).
- High cholesterol levels.
Smoking.
Early PDR
In the early stages of Proliferative Diabetic Retinopathy (PDR), neovascularization begins to form on the retina or optic disc. These abnormal blood vessels are weak and prone to leakage, leading to complications
Features of Early PDR
- New Blood Vessel Formation: Tiny, fragile blood vessels grow in areas where oxygen is lacking, typically near the retina or optic disc.
- Increased Risk of Retinal Detachment: These abnormal vessels may bleed, leading to the formation of scar tissue that pulls on the retina. This traction can cause the retina to detach, potentially resulting in severe vision loss
Diagnosis
- Dilated Eye Exam: A comprehensive eye exam allows the ophthalmologist to visualize retinal changes and neovascularization.
- Optical Coherence Tomography (OCT): This imaging test provides detailed cross-sectional images of the retina, helping assess any swelling or structural damage.
- Fluorescein Angiography: A dye is injected into a vein to highlight the blood vessels in the retina, revealing areas of leakage and abnormal growth.
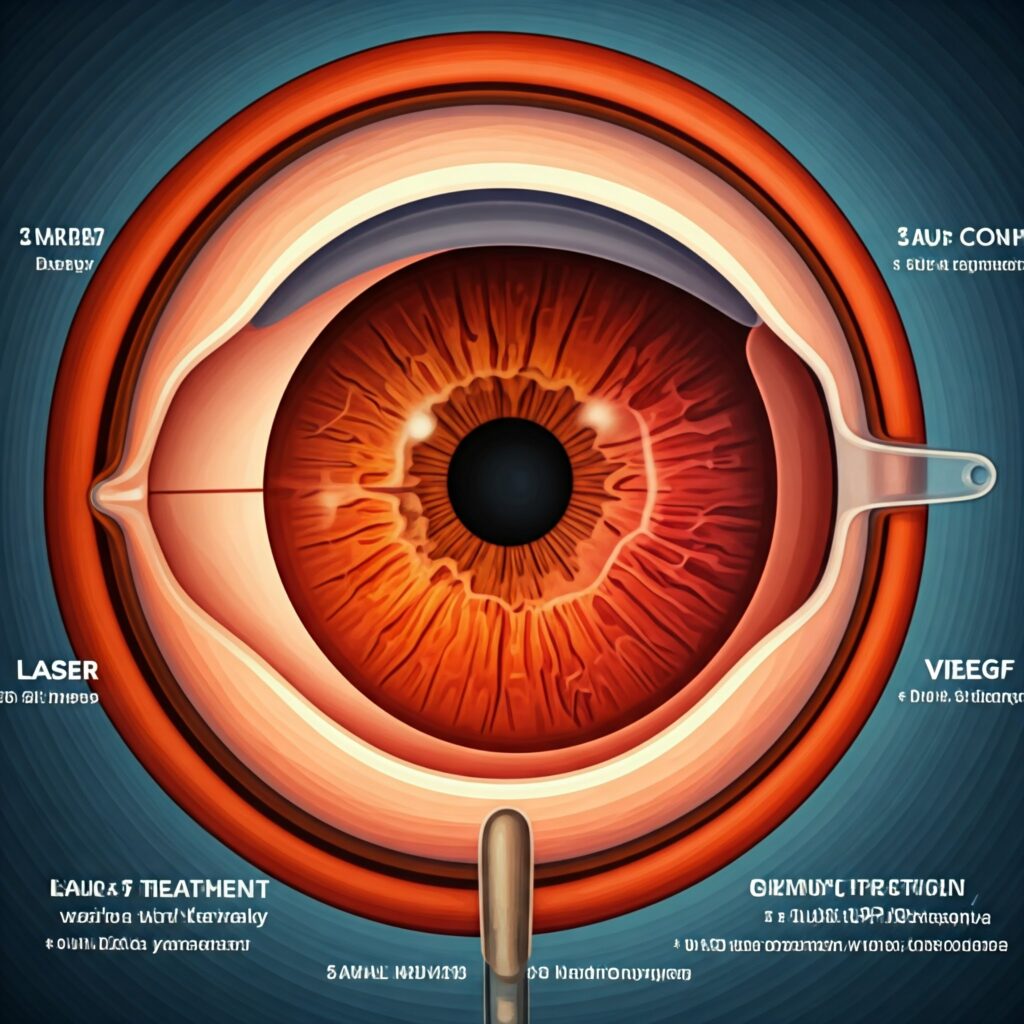
Treatment for Early PDR
- Laser Photocoagulation: This is a first-line treatment to shrink abnormal blood vessels and prevent further growth.
- Anti-VEGF Injections: Medications like bevacizumab or ranibizumab can reduce neovascularization and control swelling.
- Blood Sugar Control: Maintaining tight glycemic control is crucial to slow disease progression
Advanced PDR
When Proliferative Diabetic Retinopathy (PDR) advances, neovascularization becomes extensive, and fibrous tissue forms alongside the abnormal blood vessels. This stage is associated with a higher risk of severe vision-threatening complications
Features of Advanced PDR
- Extensive Neovascularization: The abnormal blood vessels multiply and spread, covering larger areas of the retina.
- Fibrous Tissue Formation: Scar-like tissue develops alongside new vessels, increasing the risk of retinal distortion and detachment.
- High Risk of Vitreous Hemorrhage: Fragile blood vessels can rupture, causing blood to leak into the vitreous, resulting in sudden vision loss or floaters.
- Tractional Retinal Detachment: The fibrous tissue can pull on the retina, causing it to separate from the back of the eye—a sight-threatening condition requiring urgent treatment

Diagnosis
- B-scan Ultrasound: Used when the vitreous is clouded by blood, this test helps evaluate the retina’s condition.
- Fundus Photography: Detailed images of the retina to document disease progression.
- Visual Acuity Tests: Helps measure the level of vision loss
Treatment for Advanced PDR
- Vitrectomy Surgery: This procedure removes the vitreous gel and any scar tissue, reducing traction on the retina and clearing hemorrhages.
- Laser Treatment: Panretinal photocoagulation may still be used to target new areas of neovascularization.
- Anti-VEGF Therapy: Injections continue to play a role in managing neovascularization