Evaporative Dry Eye (EDE)
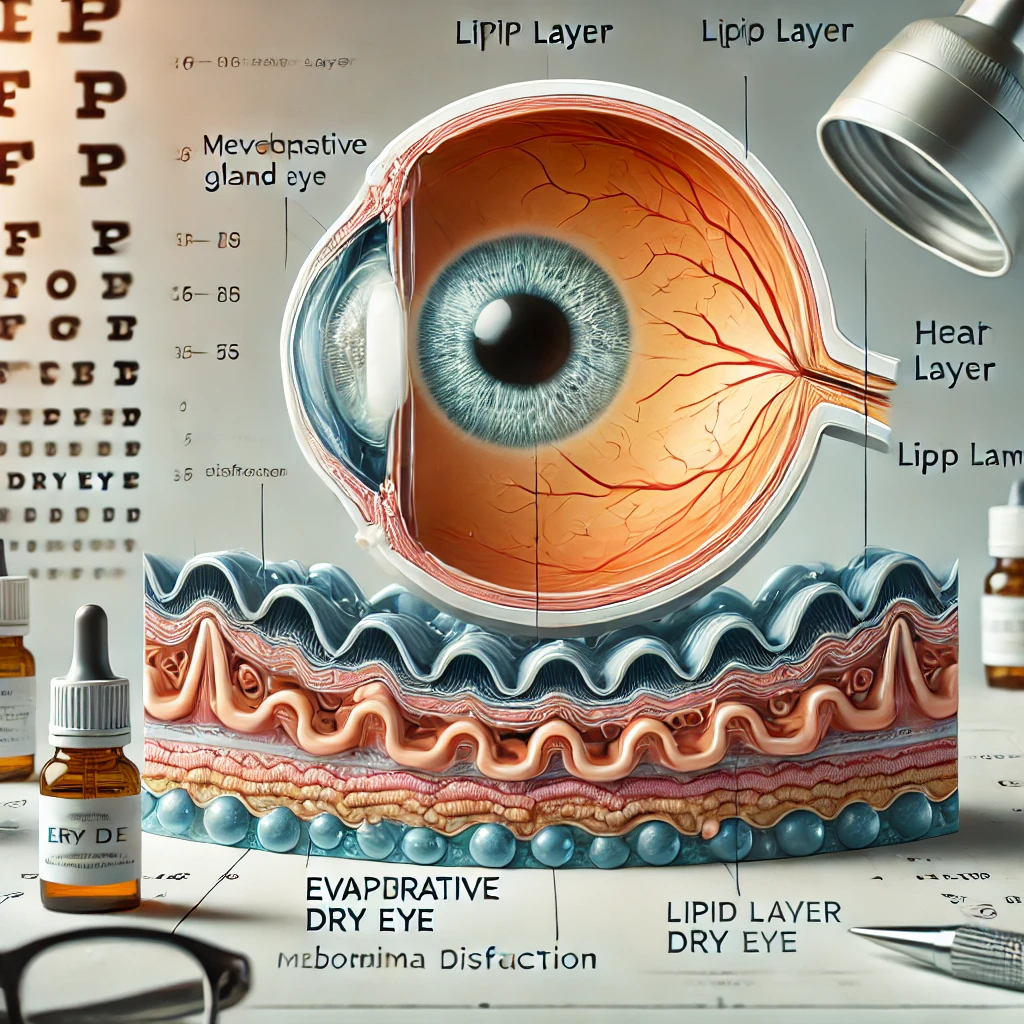
Evaporative Dry Eye (EDE) is a subtype of dry eye disease caused by excessive evaporation of the tear film, leading to instability and ocular discomfort.
Unlike Aqueous Deficient Dry Eye (ADDE), where tear production is insufficient, EDE stems from a compromised lipid layer, often due to Meibomian Gland Dysfunction (MGD) or environmental factors. This guide explores the causes, symptoms, diagnosis, and management strategies for EDE.
The tear film is a complex structure consisting of three layers: lipid (outermost), aqueous (middle), and mucin (innermost). The lipid layer, produced by the meibomian glands in the eyelids, prevents tear evaporation and stabilizes the aqueous layer.
In EDE, dysfunction or blockage of these glands leads to insufficient lipid production, resulting in rapid tear evaporation
Causes of Evaporative Dry Eye
Primary Causes
- Meibomian Gland Dysfunction (MGD): The most common cause of EDE, MGD occurs when the meibomian glands become obstructed or dysfunctional, reducing lipid secretion.
- Blepharitis: Inflammation of the eyelid margins can disrupt meibomian gland function.
Environmental Factors
- Low Humidity: Dry climates or air-conditioned environments accelerate tear evaporation.
- Wind or Dust Exposure: External irritants can exacerbate EDE symptoms.
- Digital Eye Strain: Prolonged screen time reduces blinking frequency, affecting tear distribution and lipid layer integrity
Secondary Factors
- Contact Lens Wear: Long-term use can disrupt the tear film’s lipid layer.
- Hormonal Changes: Androgen deficiencies, particularly in postmenopausal women, may impair meibomian gland function.
- Medications: Certain drugs, like isotretinoin for acne, can reduce lipid secretion.
Symptoms of EDE
Common symptoms of Evaporative Dry Eye include:
- A stinging or burning sensation in the eyes.
- Foreign body sensation, often described as a gritty feeling.
- Intermittent blurry vision, particularly during tasks requiring prolonged focus.
- Increased sensitivity to light (photophobia).
Reflex tearing, where the eyes overproduce tears as a response to dryness

Diagnosing Evaporative Dry Eye
Accurate diagnosis of EDE is crucial for effective treatment. Common diagnostic approaches include:
Patient History
- Identifying lifestyle factors, like excessive screen time or environmental exposure.
- Discussing symptoms and their impact on daily activities.
Clinical Tests
- Tear Breakup Time (TBUT): Evaluates tear film stability; a short TBUT indicates increased evaporation.
- Meibomian Gland Assessment: Includes gland expression tests and imaging to detect blockages or atrophy.
- Ocular Surface Staining: Uses dyes like fluorescein to highlight areas of dryness or damage.
Advanced Diagnostic Tools
- Lipid Layer Thickness Analysis: Measures the lipid layer’s thickness and quality.
- Meibography: Imaging technology that visualizes the structure and function of the meibomian glands.
Treatment Options for Evaporative Dry Eye
EDE management focuses on improving lipid layer function, reducing inflammation, and addressing environmental triggers.
Lifestyle and Environmental Adjustments
- Increase indoor humidity with a humidifier.
- Avoid prolonged exposure to dry, windy, or air-conditioned environments.
Practice the 20-20-20 rule during screen time: every 20 minutes, look at something 20 feet away for 20 seconds
Warm Compresses
- Regularly applying warm compresses to the eyelids helps to unblock the meibomian glands and improve lipid secretion.
Pharmacological Treatments
- Artificial Tears with Lipid Supplements: Specialized drops help restore the lipid layer.
- Anti-inflammatory Eye Drops: Corticosteroids or cyclosporine can reduce eyelid inflammation.
- Oral Omega-3 Supplements: May enhance meibomian gland function and lipid production.
Device-Based Therapies
- LipiFlow®: A thermal pulsation system that clears blocked meibomian glands.
- Intense Pulsed Light (IPL): Reduces inflammation and improves meibomian gland output.
Hygiene and Lid Care
Maintain proper eyelid hygiene with gentle cleaning agents or prescribed wipes to control blepharitis
Addressing Underlying Conditions
- Treat conditions like acne rosacea or hormonal imbalances that may contribute to EDE.
Complications of Untreated EDE
If left untreated, Evaporative Dry Eye can lead to:
- Chronic ocular surface inflammation.
- Corneal damage, including scarring and increased risk of infections.
Persistent discomfort and significant reduction in quality of life
Prevention and Prognosis
While EDE is a chronic condition, its symptoms can be effectively managed with early intervention and a consistent care routine. Preventive strategies include:
- Staying hydrated and maintaining a balanced diet.
- Protecting the eyes from harsh environmental factors with sunglasses or protective eyewear.
Limiting screen time and taking frequent breaks to ensure proper blinking
